SERVICES
- Introduction
- Dosage Charts
- Acne
- Burns
- Chicken Pox
- Colds
- Conjunctivitis
- Constipation
- Cradle Cap
- Croup
- Diaper Rash
- Diarrhea
- Earaches
- Fever
- Hand, Foot and Mouth Disease
- Head Injury
- Head Lice
- Hives
- Impetigo
- Ingrown Toenails
- Nosebleeds
- Pinworms
- Poison Ivy
- Poisoning
- Ringworm
- Ringworm of the Scalp
- Roseola
- Streptococcal Pharyngitis
- Vomiting
- Wheezing
- Yeast Infection
- Microbiology for Parents
Introduction
This page contains information on a few of the most common childhood health issues, along with treatment guidelines and information on when you should call our office. If you have specific questions, you can call our office or use our secure online portal. You can also choose the condition you want to read about from the list on the left.

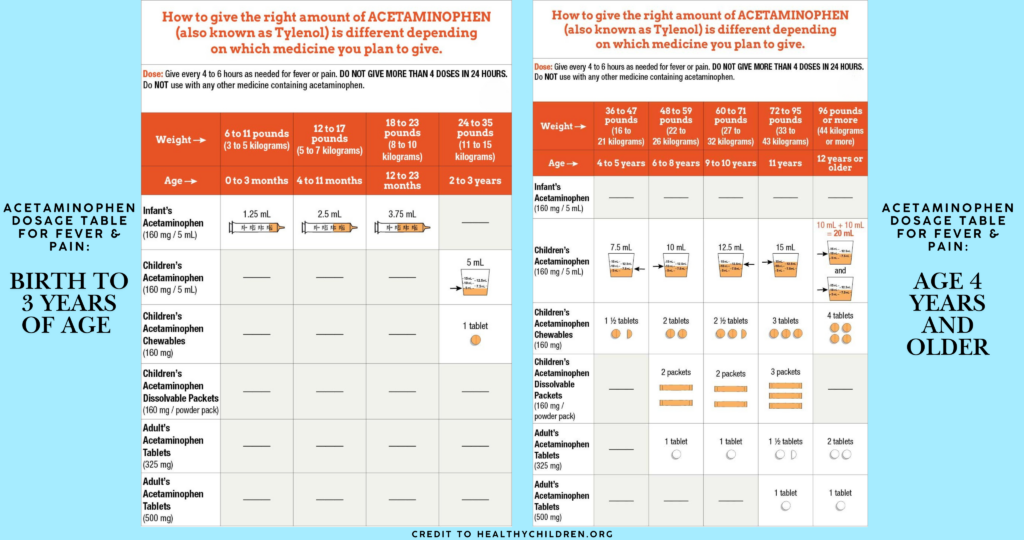
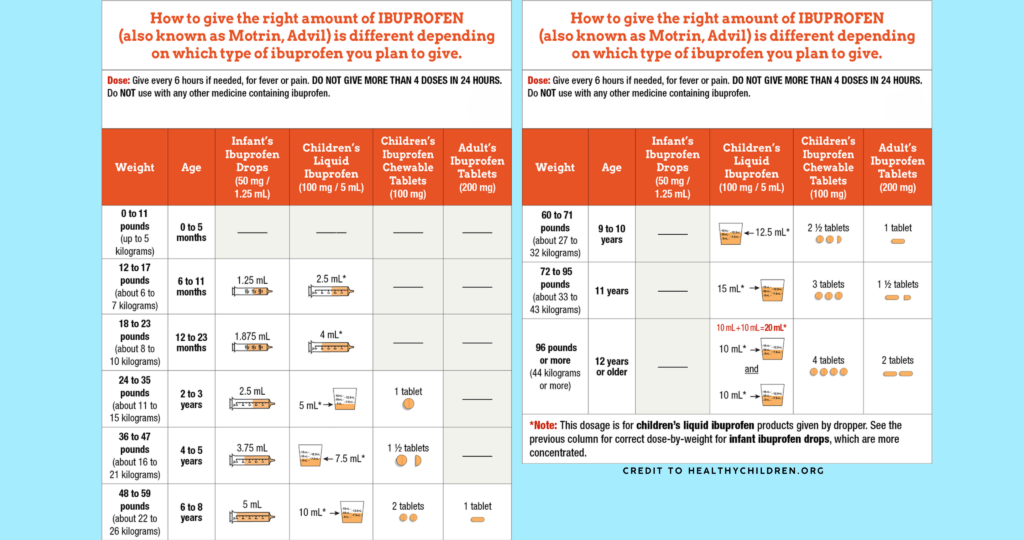
Dosage Charts
Acetaminophen (i.e., Tylenol®, Feverall®, Tempra®) is an over-the-counter medicine used to reduce fever and relieve pain. Improper dosing is one of the biggest problems in giving acetaminophen to children. These charts, based on your child’s weight, can help determine the right dosage amount, but is no substitute for your pediatrician’s advice. DO NOT USE FOR INFANTS UNDER 12 WEEKS UNLESS DIRECTED BY YOUR PEDIATRICIAN. Frequency: Every 4 – 6 hours but no more than 4 times per day.
Ibuprofen (i.e., Motrin®, Advil®) is an over-the-counter medicine used to reduce fever and relieve pain. This chart, based on your child’s weight, can help determine the right dosage amount, but is no substitute for your pediatrician’s advice. DO NOT GIVE TO INFANTS UNDER 6 MONTHS OF AGE – Frequency 6 – 8 hours
Acne
Acne is caused when pores in the skin become plugged and inflamed. It begins to occur in puberty when certain hormones in the body are increased, causing more oil gland activity in the face, back, and upper chest. The cells that line the oil glands shed and clog the pores causing whiteheads and blackheads. When the whiteheads rupture, they cause inflammation and pimples. Things that make acne worse are “popping” pimples, too much scrubbing, things that rub the skin (hats, headbands, hair), menstruation, heavy cosmetics, and in some people, stress and tension. Acne is not caused by eating certain foods or by dirt. You may inherit a tendency toward being susceptible to developing acne if other members of your family have acne. There is no cure for acne, and it can last for years although it does tend to improve over time. In order to keep acne controlled you need to have a consistent, patient, and persistent treatment plan. It takes at least 4–6 weeks to see any improvement.
Suggested Treatment for Acne
- Wash only 2–3 times per day with a mild soap using hot water to wash and cool water for the final rinse. Avoid harsh soaps or abrasives.
- Use 5% benzoyl peroxide gel or lotions. Begin with one application per day and go to twice a day after a week if your skin isn’t too red or peeling. You should apply it over the entire area where pimples may occur, not just were the current pimples are.
- Apply it 30 minutes after washing to be sure the skin is completely dry, and do not apply it to the delicate skin around the eyes, mouth, and corners of the nose.
Burns
The best treatment for burns is their prevention. The most common causes of burns in young children are: scald burns caused by hot liquids overturned by children, excessively hot bath water, and burns caused by heating elements, such as curling irons and stoves. Sunlight and certain chemicals may also cause burns. Burns are divided into three categories. First degree burns are those which are superficial causing redness but no blistering. They can be uncomfortable but seldom cause major problems. The main goal in treating these burns is the relief of pain. Second degree burns are those in which there is blistering. These burns are more serious as they can easily become infected. If well treated, they seldom lead to more than minimal scarring. Third degree burns destroy the entire thickness of the skin and are therefore extremely serious. Serious scarring can result and skin grafting may be necessary if third degree burns are present. They are less painful as the nerves are destroyed. Tylenol® or other over-the-counter pain medications can accomplish treatment for pain of burns. If a stronger pain medication is necessary, it will be likely that a physician should see your child. While no other treatment may be necessary in first degree burns, a physician should see second and third degree burns. Care should be taken not to contaminate the wound with bacteria. If the area is small, wash it gently with soap and water followed by lightly covering it with a topical antibiotic ointment such as triple antibiotic ointment. Next, place a fresh clean gauze covering on the burn and cover the dressing to prevent it from falling off. Remove the old dressing material daily, washing the wound gently and checking for signs of pus-like drainage, excessive swelling, increased redness or fever, which may indicate the beginnings of an infection. If any of these signs are present, please contact us. If there is a question about the severity of a burn, please call us to discuss the matter.
Chicken Pox
Chicken pox is an infection caused by a virus, causing rash and fever. Routine vaccination now prevents most cases of chicken pox. Anyone exposed to chickenpox who has not been vaccinated should contact our office promptly. There is often one day of not feeling well before the rash breaks out. The rash begins with red bumps that look like insect bites, which then develop into blisters containing clear fluid. The fluid may become cloudy before the blisters begin to crust over and scab. The rash can be anywhere on the skin, scalp, or in the mouth, throat, or vagina. After being exposed, the illness begins in 10-21 days and will last 5–7 days. Your child can infect others from 2 days before the rash appears until the last blisters completely scab over. Relief of itching is very important to keep your child comfortable. Lukewarm baths with Aveeno or baking soda (1/2 cup) or applying calamine lotion to the blisters can reduce the itching. Antihistamines such as Benadryl® may also provide some relief. Only acetaminophen (Tylenol®, Tempra®), not aspirin, should be used for fever. The fingernails should be kept short to avoid scratching and infecting the sores. Call the office if your child develops vomiting for more than 4 hours, persisting fever, extreme sleepiness or difficulty waking, severe cough, chest pain, or shortness of breath, severe stomach pain or if the skin around the sores becomes red, warm and tender.
Colds
A cold is a viral illness that causes a cough, runny nose, and often a sore throat. Antibiotics do not kill cold viruses. A mild cold may need no treatment. Cold medicines may help the symptoms of colds, such as runny nose and cough, but do nothing to cure the illness more quickly. Fever should be treated with an appropriate dose of fever-reducing medicine such as Tylenol® (see also the section on fevers). A runny nose can be treated with saline nose drops such as NaSal®, which may be purchased without prescription. Other than saline drops, please call during office hours before giving infants less than 6 months of age any cough and cold medications. If there is a cough, increase your child’s fluid intake, but allow the child to eat and drink any food that he desires. Vaporizers and humidifiers are occasionally helpful if the air is particularly dry, such as during the winter months. If you have used one of these and find no change in the child’s condition, there is no reason to continue its use. Cough persisting for more than a few days or cough associated with fever or chest pain should be seen by a physician. Raising the head of the bed or crib 30° or less may help your child have less nasal congestion and sleep more readily. Please call us immediately if your child has difficulty breathing (straining and pulling to get air in and out). This does not refer simply to the child sounding quite congested when he breathes. Children with difficulty breathing may breathe greater than 60 times per minute, have intercostal retractions in which the skin between their ribs sinks in with each breath, or have other signs which may make it appear that the child is in great difficulty. If a cold does not resolve within two weeks, a fever of 101°F or higher lasts 3–4 days, or the child’s nasal discharge lasts for longer than 10 days, an office visit is advised.
Conjunctivitis
Conjunctivitis is an infection or inflammation of the membranes that cover the eye and eyelids. It is uncommon in the newborn period and should be examined by your pediatrician to establish the cause of infection. Conjunctivitis is common in childhood and is frequently referred to as “pinkeye.” Redness of the eye, the lids, with swelling and a discharge is usually seen. Often in bacterial infections, the eyelids will be matted and struck together in the morning upon awakening. These infections should be seen by your pediatrician and treated with antibiotics. This is not, however, an emergency but a condition that should be attended to promptly during office hours. If there is much swelling of the lids, redness, discharge and fever, the infection may have extended deeper into the surrounding tissues and should be seen as soon as possible. Many conditions, which look similar to bacterial infections of the eyes, are due to viral infections, allergies, foreign particles or other irritants (such as swimming pool water) and do not require antibiotics. Remember that in the newborn period, many babies will have a condition know as “wet eye.” This causes a clear drainage with a small amount of mucus, but little or no redness or swelling of the lids. This is caused by a blockage (usually temporary) of the baby’s tearduct and usually is relieved by gentle massage. Do this by placing your little finger on the side of the baby’s nose, near the angle of the eye and using a rocking motion with pressure, three times a day. Occasionally, an ophthalmologist will need to see your baby if the condition persists after 12 months of age.
Constipation
Constipation does not refer to the number of bowel movements a child has in a 24-hour period, or even longer. Constipation refers to the passage of very hard bowel movements that by their dry, hard consistency make it difficult and painful for the child to use the bathroom. Although infants can appear to be straining to pass a stool, as long as the stool that results is soft, there is no constipation. Children may have stools six to eight times each day, or once every third or fourth day. As long as the stools remain other than extremely hard in consistency, there is no need to worry about any of these patterns. Constipation can be caused by diet, illness, or psychological factors. Rarely, there is a congenital defect in the large intestine which causes constipation. Adjusting a child’s diet to increase the roughage and fiber, such as providing fruit (except bananas), raw vegetables, whole grains, increased amounts of water and decreased amounts of dairy products may be all that is necessary in an older child. Adding Karo syrup, one teaspoon per two ounces of formula, to the formula of younger children may be necessary to alleviate constipation during infancy. If your child is quite uncomfortable, you may use a glycerin suppository, such as Babylax®, to help stimulate a bowel movement and relieve constipation. Consult us by phone during regular office hours before giving multiple suppositories or using other home remedies such as laxatives, enemas, or mineral oil.
Cradle Cap
Cradle cap is a harmless skin condition which is present when there are oily, yellowish scales or crusted patches on the scalp of an infant. While it is usually only present on the scalp, it may also be present on the forehead, eyebrows, and behind the ears. The best treatment for this is to use an antidandruff shampoo, such as Head and Shoulders®, once or twice weekly, taking care to avoid getting it in the eyes. An alternate treatment is to rub baby oil or olive oil into the scalp, allow it to remain there for ten minutes, remove the scales with a fine toothed comb, and then shampoo the hair. If signs of infection, such as redness or a hard, yellow-brown scabbing crust should occur, it will be necessary to have your child seen by their pediatrician.
Croup
Croup is an illness of the respiratory system, usually caused by a virus, involving the vocal cords and upper airways. It causes a barky cough, which often becomes worse at night and sounds alarming but usually is not dangerous. Your child may also have a fever, decreased appetite, and a harsh crowing sound when breathing in (stridor). Comfort and reassurance may help, as the stridor or cough tends to worsen with anxiety and activity. Home treatments that may give some improvement include taking your child into a bathroom that has been steamed for 10-15 minutes, then exposing your child to cool night air or cool air from the refrigerator. Either cool or warm mist may also help, but be sure to keep hot humidifiers out of reach of small children to avoid burns. The worst of the illness usually lasts 2–3 days, but a wet cough may persist up to 1–2 weeks. A cough suppressant can be tried to help relieve the cough. Call immediately if your child has very fast breathing, over 70–80 times per minute, bluish color to the lips, a persistent cough, difficulty breathing, or a fever of 103° or higher with croup symptoms, stridor during the day.
Diaper Rash
Diaper rashes are common in infants and can have various causes. For a mild rash, the most common cause is irritation caused by a wet diaper. This can be helped with careful cleansing when changing wet diapers and using Desitin® ointment, or A&D® as needed. Infants can also become irritated in the diaper area when having diarrhea because of the contact with the skin with multiple loose stools. If you notice this is beginning to occur, a thicker cream such as zinc oxide or one of the thick white ointments, as they are more protective and should be used (see Yeast Infections).
Diarrhea
Diarrhea refers to the passing of more than 8-10 watery stools or unusually frequent in any one 24-hour period.
What to do:
Infant:
- If breastfeeding, continue breastfeeding
- If formula feeding, Pedialyte® should be given for 6 hours. This is followed by a soy formula (e.g., Isomil® DF) for 1-2 weeks.
Older Children:
- Clear liquids for 6 hours followed by clear liquids and a modified B.R.A.T. diet (bananas, rice, applesauce, toast or crackers, pastas, or lean protein such as chicken) for 24 hours
- Return to regular diet, but limit milk or milk products (except yogurt which is a recommended food for diarrhea) for 1–2 weeks.
Call us immediately if:
- There is a large amount of blood mixed with the stool.
- Along with the diarrhea, there has been vomiting to the point that mucous membranes in his mouth are now dry and sticky and no longer moist and wet.
- The child appears especially ill, fever, cramps, vomiting
Call us promptly during regular office hours if:
- The diarrhea has lasted longer than 3 days with more than 8 stools per day.
- The fever is higher than 101° for more than 24 hours.
- There are streaks of blood in the stool.
- The diarrhea is accompanied by persistent vomiting
Earaches
Earaches are common in children and may or may not be associated with an infection of the middle ear called otitis media. Ear infections are not considered emergencies, and it can take up to three days for the discomfort of an ear infection to resolve once antibiotics are started.
There are several things you can do if your child wakes up with an earache:
- Give an appropriate dose of a pain reliever (Tylenol [acetaminophen] or if the child is 6 months or older Motrin [ibuprofen])
- Have the child sit upright for about 30 minutes
- Have the child take a drink, which may equalize pressure on both sides of the eardrum
Fever
A fever is a temperature of 100.4° or greater rectally. Temperatures normally vary during the day. Children can have temperatures up to 100° as a normal variation. Fever is a symptom of an illness and finding the cause may require a visit to the office. If your child is less than 2 months old with a fever of 100.4° or greater, please call our office before administering any medication. A rectal temperature is most accurate since it picks up temperatures from the body’s core.
What to do:
- It is not necessary to treat a temperature less than 102°, unless the child is uncomfortable
- For a temperature of 102° or more, or if the child is uncomfortable, give Tylenol or some other form of acetaminophen (see dosage chart). You may also give Motrin or ibuprofen if the child is 6 months or older (see dosage chart).
- Encourage fluids
- Keep the child cool
- Use a minimum of clothing; keep the house cool; if temperature is 104° or greater, sponge bathe or bathe the child in lukewarm water for 10-15 minutes.
Call us immediately if:
- The fever is 105° or higher after fever-lowering medicine has been given or the child is less than 6 months of age
- He looks and acts extremely ill (i.e., is difficult to arouse, refuses to eat, is disinterested in playing, speaks without making sense, or appears extremely sick after fever-lowering medicine has been given.)
- The fever is greater than 100.5° in an infant less than 2 months of age.
- The child has a convulsion for the first time (body stiffness, eyes roll, limbs jerk)
Call us promptly during regular office hours if:
- The fever is greater than 101° for more than 24 hours and your child is under 1 year of age
- The fever comes and goes, but other symptoms are present for more than 3 days
Hand, Foot and Mouth Disease
Hand, foot and mouth disease (Coxsackie A Virus) is an infection that occurs mainly in children between 6 months and 4 years of age. It has no relationship to hoof and mouth disease of cattle. The symptoms are a low-grade fever, 100° to 102°F (38° to 39°C); small, usually mildly painful ulcers in the mouth, and small water blisters or red spots on the palms and soles, and on the webs between the fingers and toes (five or fewer blisters per limb). Small blisters or red spots may also appear on the buttocks or lower legs. The fever and discomfort usually disappear in three or four days and the mouth ulcers usually resolve in seven days, but the rash on the hands and feet can last 10 days. Hand, foot and mouth disease is quite contagious and usually some of your child’s playmates will develop it at about the same time. The incubation period after contact is three to six days. Your child may return to school or day care when the fever returns to normal. Most children are contagious from two days before the rash appears until two days after it disappears.
Home care instructions:
- Offer a soft diet for a few days and encourage your child to drink plenty of clear fluids. Cold drinks, ice pops, ice cream and sherbet are often well tolerated.
- Do not give your child citrus fruit, salty foods or spicy foods. They will further irritate his mouth. Also avoid foods that need much chewing. For infants, you may try giving liquids by cup rather than a bottle because the nipple can cause pain.
- Give acetaminophen or ibuprofen if necessary. Acetaminophen or ibuprofen may be given for a few days if your child’s fever is above 102° F (39° C) or the mouth ulcers are very painful. (See also the section on
Head Injury
Head injuries are very common in children. Most head injuries are not serious; however, if your child does have a blow to the head, there are some things to look out for. Complications of head injuries include: concussion, which is a temporary problem with brain function but no actual brain injury; skull fracture; loss of consciousness; headaches, internal bleeding.
Signs to watch for that may indicate a complication of head injury include:
- Persistent nausea or vomiting
- New drainage of clear or bloody fluid from the nose or ears
- Persistent headache or dizziness
- Seizure
- Labored breathing
- Difference in pupil size or pupils that do not get smaller when a bright light is shined in them
- Excessive sleepiness or a change in behavior.
Head Lice
Lice are small, grayish-tan, wingless insects that live in the hair, feeding off the scalp. If your child comes home with head lice, don’t panic. Millions of children contract lice each year. Children play in close contact with one another and exchange things such as hats, clothing, brushes, combs, pillows, and other personal items which can result in transmitting head lice from one child to another. They can be easily and effectively treated with cream rinse or shampoos to kill the lice and their eggs (nits). To examine for head lice, carefully examine the hair and scalps of all family members for lice and their eggs. While the lice are small, grayish-tan, wingless insects that you can see on the scalp or one of the hair shafts, the lice eggs (nits) are small, white specks which are found firmly attached to the hair shafts, usually close to the scalp. These are usually found at the nape of the neck and behind the ears. If you find lice or nits, again don’t panic. This is not an emergency situation. Nix Cream Rinse can be purchased over-the-counter at your local pharmacy. Follow the directions on the package and do not repeat treatment more frequently than every 7 days. After using the cream rinse or shampoo and drying the hair thoroughly, the nits may be removed with a special nit comb. Combing to remove the nits is not absolutely necessary, but should be done for cosmetic reasons. Some schools have a no nit policy, which prevents children from returning to school until their hair and scalp reveals no nits. The American Academy of Pediatrics does not feel this is necessary. To prevent spreading lice from one person to another, make sure people with head lice do not share articles such as combs, brushes, towels, hats, scarves, pillows, etc., that have come in contact with their head, neck, or shoulders. Use hot water to wash lice-exposed clothing, towels, and bed linens. Soak combs and brushes in hot water for 10 minutes. Dry clean hats and clothing that cannot be washed or seal them in a plastic bag for at least two weeks. Vacuum carpets, upholstery, pillows, and mattresses, which may have been exposed to the person with head lice. Be on the lookout for signs that indicate that other members of your family have been infected or that the child has become infected again. The most common symptom is severe itching on the back of the neck and head. If you notice your child scratching excessively in this area, check his/her head for nits and lice. Again, if nits or lice are found, don’t panic. Follow the directions carefully on the over-the-counter products to remove lice, especially for the frequency of application of shampoo. As these head lice medications have been used for some time, some resistant head lice strains are out there. If after following the directions on the package lice are still alive, then an application of thickly applied mayonnaise or olive oil overnight with a plastic shower cap over the hair should smother them. Wash out the application in the morning and again comb nits out with a fine toothed comb.
Hives
Hives or urticaria is a rash characterized by large areas of raised, slightly reddened swelling (welts), which frequently occurs as an allergic reaction.
Common causes include:
- medications (both prescribed by your physician and purchased over the counter)
- foods (especially shellfish such as shrimp, nuts, eggs, strawberries, tomatoes)
- plants
- pollens
- animal dander
- chemicals (including those used at home and work and cosmetics)
- insect bites or stings
- infections (especially viruses)
- and occasionally causes such as heat, cold, sunlight, stress or certain rare diseases.
Impetigo
Impetigo is a skin infection caused by bacteria. Impetigo can look like crusted, scabbed areas of skin, especially with yellow honeycomb appearing scabs, or can be areas of large blisters that pop leaving large, round areas of red, raw skin which progressively increase in size and spread. Occasionally, impetigo can look like pus-filled pustules or blisters. Contact with the sores or with the fluid draining from them can lead to the infection spreading to other sites and to other people. The initial treatment for impetigo is to keep the skin area clean and dry by soaking the area well with soap and water, removing the scabs. Keep the infected area open to air; if necessary, cover it with a bandage to prevent scratching. A simple area of impetigo can sometimes be treated with a topical antibiotic such as a triple antibiotic ointment available without a prescription. If several areas are present or the area of infection is large, impetigo is best treated by an oral antibiotic that can be prescribed after seeing your child. Any areas of skin infection with large areas of surrounding redness or accompanied by a fever of 101° F or greater should be seen by a physician.
Ingrown Toenails
Tenderness, redness, and swelling of skin surrounding the corner of the toenail on one of the big toes is an ingrown toenail.
Prevention includes:
- Avoiding tight fitting or narrow shoes.
- Cutting the toenails straight across, leaving the corners. Do not cut them too short.
Treatment:
- Soak feet twice a day in bathtub.
- Let foot soak in water and bacterial soap.
- While the foot is soaking, massage outward the swollen part of the cuticle.
- Use an antibiotic ointment (i.e. Neosporin). If the cuticle is just red and irritated, an antibiotic ointment is not needed. If cuticle becomes swollen or oozes secretions, apply an antibiotic ointment 5-6 times a day.
Nosebleeds
There are many tiny blood vessels within the lining of our nose. Low humidity, frequent nose blowing, picking the nose, or blows to the nose can irritate these blood vessels and cause bleeding. For frequent nosebleeds, a small amount of Vaseline used inside the nose 1-3 times daily should help. If your child’s nose begins to bleed, have him/her sit upright on your lap or beside you. Pinch the nostrils together gently for 5 minutes to allow a blood clot to form. Although it is tempting, do not peek to see if the bleeding has yet stopped, as this will break any clot that is forming. After pinching the nose together for 5 minutes, remove your hand to see if the bleeding has stopped. If the bleeding continues, again try pinching the nose closed gently for an additional 5-minute period. If bleeding persists longer than 30 minutes, please call us.
Pinworms
Pinworms are small, white, thin, straight, pin-sized worms which inhabit the rectum and the colon. They emerge during sleep onto the perianal skin causing intense itching. There are no adverse effects from pinworms other than possible mild vaginitis or vaginal inflammation caused by their itching in girls. Pinworms can be acquired by acquiring eggs from the skin during scratching and transferring them to the mouth. They may also be swallowed when inhaled while handling clothes and bedclothes of infected individuals. If your child exhibits marked anal itching, it is not unreasonable to check for pinworms. Pinworms are easily treated with oral antiparasitic medicines including Pin-X, which is available over the counter. It is often necessary to treat each member of the family, although pregnant women should not take this medication. While pinworms can be quite annoying, they are certainly not life threatening and not an emergency situation.
Poison Ivy
Poison ivy or contact dermatitis, as it is also called, is caused by contact with the oil of the poison ivy plant or similar plants whose chemicals cause a blister-like itching rash. Poison ivy can occur only after actual contact with the sap of the plant or form the smoke of a burning plant. Once it has been bound to the skin it cannot spread to other sites, although other areas of poison ivy may become apparent over the next one to two days. It is possible to contact additional sap from clothing that has sap on it and has not yet been washed. The obvious best treatment is prevention of contact with poison ivy plants or similar plants. If you do accidentally come in contact with the plant, wash the involved skin and clothing immediately. Treatment involves applying cool compresses made by soaking gauze pads or washcloths in Burrow’s Solution which can be obtained at a local pharmacy. It is helpful to do this three or four times daily. Calamine lotion, Caladryl Clear, or Cortaid can also be applied to relieve itching and hasten healing. Oral Benadryl, one teaspoon for every 25 pounds of body weight, can be given every six hours for itching. If these measures fail to relieve itching or control poison ivy, or the rash involves the face, please call our office. If there is fever, excessive swelling, pain, redness, or pus-like drainage from the area, please call our office.
Poisoning
Toddlers and preschoolers are quite curious. Because of this, they often find innovative ways to get into prescription medicines, household products and plants that are poisonous. Prevention is always our main goal. By 8-9 months it is important to have household cleaning products, household detergents and other household aids such as dishwasher detergents put up far out of reach of the infant. This is best done by putting them in secure spots that are both out of the reach of the child and locked to prevent access. Local hardware stores carry a wide variety of latches for cabinets which are quite useful for the young child. It is also important to store products in the original container. Things such as motor oil, gasoline, and other outdoor products should never be left at a height a child could easily reach, nor should they be left in non-original containers such as putting gasoline in Coke bottles.
If your child has gotten into something which you are afraid may be poisonous, do the following:
- If possible, have the original container at hand, keeping it with you as you seek help.
- Call Poison Control at 404-616-9000 (metro Atlanta) or 1-800-282-5846 (throughout Georgia).
- If your child is blue, has difficulty breathing, or is lethargic, Dial 911 to summon an ambulance.
- Remember to take the original container of the product swallowed by the child with you to the emergency department.
Ringworm
Ringworm is a lesion that is generally pink, scaly, and ring-shaped, with a raised border and clear center. The patch of skin is usually 1/2 – 1 inch in size and mildly itchy. Ringworm is caused by a fungus infection of the skin often transferred from puppies or kittens. It is not contagious enough to worry about. After 48 hours of treatment, it is not contagious at all. It is not necessary to miss any school or daycare. If the lesion is on a hairless surface, buy Lamisil, Lotrimin or Mycelex cream. Apply the cream twice daily to the rash and 1 inch beyond its borders. Continue this treatment for one week after the ringworm patch is smooth and is gone. Encourage your child to avoid scratching the area. Call our office during normal office hours if ringworm is unimproved after 2 weeks of therapy.
Ringworm of the Scalp
Ringworm is generally on the scalp or a hairy skin surface. It is characterized by round patches of hair loss that slowly increases in size. The scalp may have scaling and usually occurs in children ages 2-10. Ringworm is a fungus and not a worm. It infects the hairs causing them to break. This is usually transmitted from other children sharing combs, hats, brushes, barrettes, pillows, and bath towels. Less than 10% of cases are caused from infected animals. Ringworm of the scalp is not dangerous but can spread. Hair growth is normal after treatment, but may take 6-12 months to recover. Call our office during normal office hours if you find evidence of scalp ringworm.
Roseola
Roseola is a common illness in children between the ages of 4 months and 2 years. It is caused by a virus, Herpes virus 6, which is related to but different from other Herpes viruses. Roseola begins with a high fever (103-104° F) for 3-5 days. After the temperature drops to normal the child develops rash that consists of small pink spots mostly over the neck, chest, and body. The rash is usually very faint but can get heavy; it lasts about one day. The diagnosis of Roseola is often not made until after the characteristic rash appears. The most important way to make your child feel better is keeping the fever down. Please see the fever section of this book for advice about lowering fever. Please call the office if your child has excessive sleepiness or irritability, persistent vomiting, diarrhea, cough, pain on urination, if the fever lasts for more than 5 days, or a sore throat is associated with the rash.
Streptococcal Pharyngitis
Vomiting
Vomiting in children is most often due to an intestinal virus. Most viruses are accompanied by diarrhea. Vomiting with an intestinal virus seldom lasts longer than 24 hours. If your child develops nausea and vomiting, provide them with frequent small amounts (1-2 tablespoons every 15 minutes) of clear liquid such as Pedialyte. When your child has had no vomiting for 6 hours, you can start solids beginning with easily digested foods such as crackers, soup, and toast. Call us immediately if: the material vomited is bright yellow or pea green in color on more than one or two occasions; the vomit contains a moderate to large amount of blood; the child is very sleepy and difficult to arouse, especially if he has a high fever; there are signs of dehydration, such as dry sticky tongue and mouth. Vomiting which has lasted less than 24 hours is not usually associated with severe dehydration, the younger the child the more rapid the dehydration. Call us promptly during regular office hours if your child otherwise appears well, but the vomiting has lasted longer than 24 hours.
Wheezing
If your child is having great difficulty breathing and is straining and pulling to get air in and out, please call us immediately or go directly to the emergency department.
What we need to know:
Has the child had any history of wheezing or asthma? Does anyone else in the family have asthma or lung problems? Is he having difficulty breathing (straining or pulling to get air in or out)? Does he have a cold?
Call us immediately if:
He has a high fever accompanying his wheezing. He is straining and pulling to get air in and out. He has swallowed any coins or other objects just prior to wheezing.
Call us promptly during regular office hours if:
The wheezing has lasted longer than 8 hours, even if there is no difficulty breathing. The fever is higher than 101° F for more than 24 hours.
Yeast Infection
Yeast infections are a very common cause of a beefy red diaper rash that can often cover the entire diaper area. Infants under 3 months of age can often develop a yeast infection with no apparent cause. In older infants, toddlers, and young children, the treatment of a bacterial infection with oral antibiotics can cause yeast to overgrow in moist dark areas such as the diaper area. Yeast may also appear in the mouth as white patches on the tongue or inside the cheeks, which do not scrape off as milk curds would. This condition is called “thrush.” If your child has thrush, call the office. We can prescribe a medication. You will also need to boil all pacifiers and nipples daily. If you are breastfeeding and your baby gets thrush, you will also need to be treated so that you are not passing the infection back and forth.
If you notice the diaper rash described above, things to do include:
- Change diapers frequently and keep the areas as dry as possible, but do not use powders or cornstarch.
- Clean the diaper area with warm water or Cetaphil cleanser with each diaper change.
- Eliminate rubber pants for infants and use only white cotton pants for toddlers or young children.
- Buy Lotrimin AF and apply 3 times daily.
Microbiology for Parents
Viruses
Because viruses are completely different types of microorganisms, antibiotics do not work to kill them. There are very few viruses that we have medicines for at this time (influenza and severe herpes virus infections are two exceptions.) There are vaccines that prevent certain viral infections (polio, measles, mumps, rubella, chicken pox, hepatitis A and B). The majority of acute illnesses that children get are viral in origin. The viruses eventually are managed by the immune system and the illness is over. In other words, we have to let it “run its course.” Common viral infections are usually not serious but can make children feel quite ill for several days. There are also rare times that viruses do cause serious illness or complications that can be severe. There are hundreds of types of viruses. Some commonly known ones are listed below.
- Parvovirus — Causes Fifth Disease
- Adenovirus — 37 human types. Causes eye infections, cold symptoms, sore throat
- Herpes — Roseola, chicken pox, HSV I mouth ulcers, CMV, EBV (mononucleosis).
- Picorna — 1 subtype called rhinovirus has at least 100 common cold strains. Enteroviruses are in this group including Coxsackie (hand-foot-mouth syndrome). Enteroviruses can cause fever without other symptoms, vomiting and diarrhea, stomach pain, cold symptoms, sore throat, eye infections, and rashes.
- Reovirus — Rotavirus
- Corona — Some colds
- Orthomyxo — Influenza A and B
- Paramyxo — 3 strains of parainfluenza which can cause croup, pneumonia, metapneumovirus
- Rhabdo — Rabies
